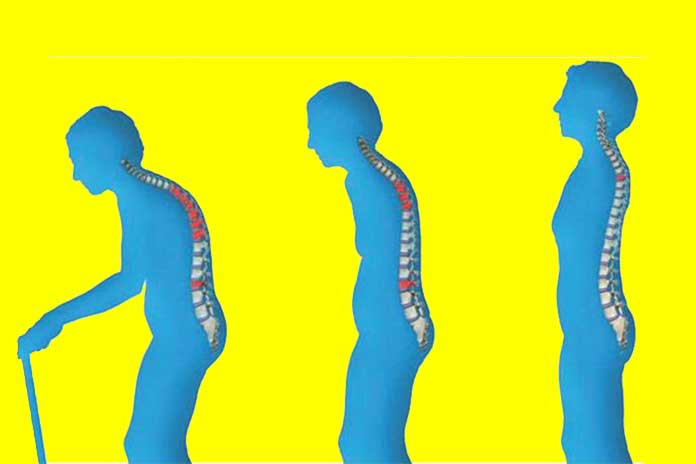
Let’s see how proper nutrition helps prevent this chronic disease that alters the structure of the bones. What is Osteoporosis? Osteoporosis is a chronic disease that alters the bone structure and reduces resistance to ‘mechanical load,’ increasing the risk of fractures. Women, in particular, suffer from it because osteoporosis is also linked to the drop in estrogen that occurs during menopause, which is essential for bones and the absorption of calcium.
But there are other risk factors, including smoking, genetic predisposition, hormonal changes (early menopause, hyperthyroidism, amenorrhea for long periods), low calcium and vitamin D intake, excessive alcohol consumption, excessive salt consumption, inactivity, low bone density, and long cortisone treatments.
Table of Contents
How To Prevent It?
What can we do to prevent it? It is very important to follow a correct lifestyle, that is:
- Adopt proper nutrition
- Practice physical activity regularly
- Not smoking
As for nutrition, the most important thing is to ensure a high quantity of calcium and all the nutrients that favor its absorption (vitamin D, K and C, magnesium, and phosphorus).
Recommended Foods
- Milk, yogurt, fresh and aged cheeses;
- Large leafy vegetables, such as artichokes, rocket, chicory, kale, broccoli, green radicchio, chard, turnips, and cabbage
- Fruit, both fresh (especially citrus fruits) and dried;
- Legumes;
- Fish and especially blue fish, such as anchovies, sardines, salmon, tuna, and so on;
- Waters rich in calcium
Also Read: How Blisters Are Treated
Foods To Eat In Moderation
- Coffee
- Alcohol
- Tea
- Red meat
- Cold cuts and salami
- Carbonated drinks
- Processed foods and canned fish
- Salt and foods rich in salt
- Vegetables and other oxalate-rich foods, such as spinach, rhubarb, parsley, tomatoes, grapes, plums, chocolate
- Whole foods or high-fiber supplements
Caution
- Avoid the intake of foods rich in calcium together with foods rich in oxalates because these substances would prevent their absorption. E.g., combining cheese and spinach means wasting part of the calcium contained in the dairy product.
- Reduce the use of table salt and sodium-rich foods (sausages, bouillon cubes, canned or pickled foods): excess sodium increases calcium loss in urine.
- Avoid consuming a high amount of protein because they increase the elimination of calcium in the urine.
- Please do not overdo it with whole foods or foods rich in fiber because the right amount is healthy, but they can reduce calcium absorption.
- Limit alcohol because it decreases calcium absorption and reduces the activity of cells that “build bone.”
Nutritional intervention must be considered a preventive or supportive tool for pharmacological intervention. In cases of osteoporosis, drug therapy must be accompanied by a diet that provides a good supply of calcium to make the therapy more effective, limit the number of supplements, or even make their use useless.
Now let’s see how much calcium and vitamin D needs to be during the day:
- Calcium: for women over 50, it is 1.2-1.5 g / day, while for men over 60, it is 1 g / day;
- Vitamin D: values equal to or greater than 20 ng / mL (50 nmol / L) are considered sufficient in the general population, but levels equal to or greater than 30 ng / mL (75 nmol / L) are recommended in the presence of the following risk conditions and diseases (such as osteoporosis, for example).
Habits Of Daily Life As Real Treatments
As mentioned before, the role that physical activity and daily life habits play should not be underestimated. Drinking too much alcohol and coffee can impair calcium absorption and increase its excretion via urine, respectively. Instead, it has been shown in numerous publications that the nicotine contained in cigarettes can anticipate menopause by up to 2 years, also bringing with it all the hormonal consequences typical of this phase of life that strongly impact the state of health of the bones.
Still, about life habits, in elderly patients who have osteoporosis, a physical activity aimed at improving the clinical condition and supervised by specialists can be helpful. In these circumstances, a moderate weekly physical activity of 150-300 minutes is recommended, accompanied by stretching and muscle toning sessions. Several studies have highlighted how physical activity exercised in these conditions allows improving bone density and functional mobility in the elderly with a decrease in falls from 25% to 50%.
Also Read: Gastric Reflux: What To Eat?